06 July 2015
•6 minute read
Cancer Screening - What You Need to Know Before You Start
Cancer is a leading cause of concern for us as we plan our futures. It is now almost a household word, most of us having in some way or other been affected by this dreaded disease. The fear is not misplaced.
Cancer is the leading cause of death in a number of developed countries with populations similar to ours including Singapore and Hong Kong. In Malaysia, since 2012, the ministry of health has noted that cancer is the second commonest cause of death in private hospitals, responsible for a quarter of total deaths per year. Cancer treatment outcomes in Malaysia are not great, largely due to the late presentation of the disease. And yet, in developed countries like Singapore, the United States and Europe, cancer cure rates are improving yearly. The difference is diagnosis at an earlier stage. The Japanese for example, have struggled with stomach cancer for decades, but treatment outcomes are extremely good as the tumors are diagnosed early following nationwide endoscopic screening.
Cancer prevention is the best way to reduce the threat of cancer. There are several modifiable risk factors which when addressed, can sharply decrease the likelihood of getting cancer. Chief among these are smoking and obesity. Efforts to educate and spur those at risk to action are on-going. These must be emphasized and inculcated into the way we think. A healthy life style is not an event, it is a habit. Nevertheless, despite our best efforts, there remain a large number of us who will be affected by this disease on account of “unmodifiable” (read genetic) factors.
Clearly the key to successful outcomes with cancer is early diagnosis. The problem with cancer is that in most cases, in early stages of the disease, one is not sick. There are no symptoms. The only way to detect these tumors early is to perform screening tests before the symptoms develop while one is apparently healthy.
Cancer screening tests are misunderstood. Except in a few types of cancer, you cannot screen for cancer using a blood test alone. This simply does not work. For example, the carcino embryonic antigen (CEA) often used to screen for colon cancer is not accurate enough to detect early colorectal cancer. This means that a negative result does not mean that you do not have the disease. Clearly, if you are concerned about having cancer, you need better accuracy.
The truth is better tests are available, there are many tests but the best test for you will depend on your risk for developing cancer. Risk assessment for developing cancer is based on a number of factors. Different cancers have different predispositions. Cancer is a genetic disease in the sense that gene mutations are the primary triggers. However, the mutations are just as likely to be somatic rather than germ line, which means you do not pass this risk down to your kids. Rather the effect of your environment has instigated the disease in you.
As such, start cancer screening with a visit with a consultant experienced in the diagnosis and treatment of cancer. This usually will comprise a detailed interview regarding lifestyle and family history. A suitable screening test can then be discussed. This may involve specific tests which need to be performed by trained professionals. This is currently the only way to get the desired outcome in the treatment of a disease as inevitable as cancer. The aim after all, is to provide peace of mind so that you may confidently plan your future without anxiety.
Cancer screening explained:
The process of screening for cancer comprises 3 steps:
- Consultation, Physical Examination and preliminary tests.
The purpose of this is to bring you face to face with information you need before screening for cancer. This is because screening is not a straight forward exercise. There are caveats you must understand and accept before proceeding. We are estimating and evaluating risks that may have a serious effect on your health. A complete consultation allows your doctor to determine if you do indeed require formal cancer screening and it may be reassuring to you to find out that you really do not. - Risk assessment and Screening protocol
Risk factors for developing cancer are identified from large epidemiological studies. More often than not, they are based on populations different from ours. For example, the risk assessment tool available on the National Institutes of Health (NIH) website for risk of breast cancer is based on Caucasian patients and cannot be directly applied to a typical Malaysian population.
Source: http://breast-cancer.ca/images/survivalstageschart.jpg
Chart Showing Improved Cancer Survival When Diagnosed at An Earlier StageAnother contentious issue in risk assessment for cancer is that the risk is often relative. A smoker is often quoted to be 23 times more likely than a non-smoker to develop lung cancer. This sounds like a large number but the actual risk of a non-smoker is about 50 per 100 000 person-years. For a smoker? About 1200 per 100 000 person-years. The risk per year is still small but increases in time.For these reasons, it is vital to have your risk assessed and explained to you by a professional before you embark on screening.
A variety of screening tests for the most common cancers have been identified. Each test comes with a degree of accuracy which has to be balanced with the degree of cost and risks. The aim is always to identify cancer while it is small and treatable which, if you did already have the disease, would lead to the best possible outcome.
- Risk reduction advice and action
Professional advice regarding risk reduction is sometimes considered a no brainer – telling you to stop smoking to cut down your chances of dying of lung cancer is hardly rocket science. However you may want to know how to quit smoking, you may want to know that you have pharmacological options that have been proven to help you quit smoking. You may also want to know 10-15 percent of non-smoking persons diagnosed with lung cancer report exposure to second -hand smoke.Sometimes, risk reduction may involve serious, drastic measures. A recent example is surgical removal of breasts followed by surgical breast reconstruction as in the case of Angelina Jolie, the well-known celebrity. Clearly this was decision that was made using the best available information in order to prevent what was almost a definite diagnosis of breast cancer in the future. Drastic, yes but the most effective way to prevent an almost certain threat to life.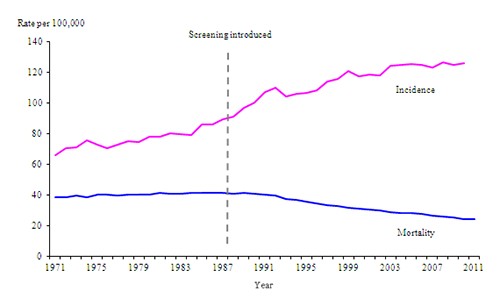
Source: http://www.ons.gov.uk/ons/resources/sbreastcancerimage2010_tcm77-280705.png
Chart Showing Mortality from Breast Cancer Dropping by Half After Breast Screening Commenced in UK
What about a full body scan?
Screening aims to reduce your chances of dying of cancer. However, it is impossible to screen for all possible sites of the disease. Today we have the means to look inside the human body entirely. We even have the means to look for the biological activity of cancer cells which is by itself like a fourth dimension in cancer diagnosis. This technology is known as Positron Emission Tomography (PET) and it involves using radioactive molecules which are metabolized by cancer cells differently compared to normal cells. When combined with Computerized Tomography (CT) scanning, the end result is as close to a whole body scan for finding cancer as can be. Unfortunately the technology is not yet perfect in that there is a risk of identifying lesions which mimic cancer but really are not. This may lead to unnecessary invasive procedures to clarify matters. Furthermore, the radioisotopes used in this procedure are prohibitively expensive. It is therefore unlikely that PET scans can be used for routine cancer screening at this time.
Screening for cancer needs to be individualized. A systematic effort to identify your risk of developing cancer, with specific tests focused on these risks will achieve the desired effect, which either an early diagnosis and hence, a better chance of cure or, quite simply, peace of mind.
For example, A 50 year old lady who smokes 1 packet of cigarettes a day for the last 20 years. She has a sibling who had breast cancer which was diagnosed at the age of 34. She is otherwise well. Her preliminary blood tests detected a blood hemoglobin level of 10.5 g%. No other abnormalities were detected.
This patient’s present clinical condition and living environment puts her at risk for a number of common cancers. She is at risk of developing lung cancer, breast cancer and there is a chance that she may already have colonic cancer. It would be wise if she underwent a low dose CT Chest, Mammography and had a stool test for occult bleeding. These tests have a very high chance of detecting cancer (a positive stool for occult blood will require a colonoscopy to detect the underlying colorectal cancer). Similar tests done yearly will decrease her chances of dying from cancer related illness. This is not to say that these tests are completely foolproof as there is a small chance one can be affected in between testing or tests may be incorrectly interpreted, one may also be inflicted by a kind of cancer that these tests are not designed to diagnose. However, the chances of missing a cancer with these tests are much less than they would be with other kinds of tests. This is described as these tests having a high sensitivity for the kind of cancer tested for. With a regular follow up, it is likely that early symptoms of any cancer will be recognized sooner.
Some tests used for screening have risks of their own. For example, use of CT scans for screening comes with a small risk of developing cancer on account of radiation exposure. With modern multi-slice scanners this risk is decreasing. However, each of us will have to be convinced of the benefit of these tests in the long run as these are stacked against such risks.
Risk reduction advice for our patient would start with advice on the various methods available to assist one to stop smoking. This can include behavioral changes and nicotine replacement. Detailed genetic counselling and testing for mutations that are known to be associated with cancer is another option that can discussed. These tests are available but require professional interpretation. Our patient should be advised to keep her weight in a healthy range and would do well to take a diet rich in vegetables and fruits while avoiding red meats.
In another example, Mr. Y is a 42 year old man with no certain evidence of cancer in the family. However he suspects 2 of his elder brothers had bowel cancer as they had passed away due to abdominal symptoms before 40. Mr. Y has a good appetite and is overweight.
International guidelines are clear that if there is a history of colorectal cancer in one’s immediate family, then you are at increased risk for the disease. However, in Mr. Y’s case a doctor will have decide on the likelihood of his suspicion. If it seems very likely, then Mr. Y should undergo colonoscopy – an invasive procedure whereby a fiber-optic endoscope is passed along the length of the colon through the anus. This procedure will detect and can confirm any cancerous or ‘precancerous’ tumors in the colon with certainty. Another option could be a less invasive fecal occult blood test and sigmoidoscopy which may be the right option if the family history is in doubt.
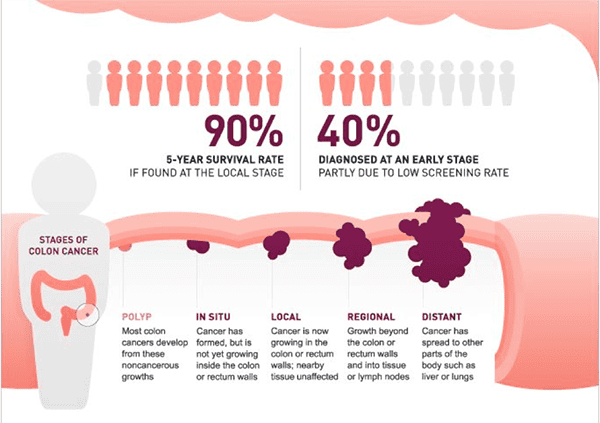
Source: http://cdn2.hubspot.net/hub/365322/file-678283347-png/colon-cancer-stage…
Illustration Explains the Evolution of Colorectal Cancer and Better Survival with Earlier Detection
As such it is clear that cancer screening in this case is not straight forward and to obtain the best result, an experienced clinical decision must be made so that early cancer is diagnosed without unnecessary added risks to Mr. Y.
Risk reduction for Mr. Y would emphasize on his increased risk for developing bowel cancer. Modifiable risk factors like obesity should be addressed- a suitable weight loss program can be suggested. A dietician may be able to help outline a diet which may help decrease the risk of cancer and lead to weight loss. If the colonoscopy shows evidence of precancerous tumors such as adenomas, endoscopic removal of these lesions may prevent cancer. Moreover, the option of starting aspirin, a cost effective, well known drug which has been shown to reduce cancer risks, can be discussed.
For Mr. Y, a proper cancer screening may be the difference between a life cut short by a unrelenting disease and a life lived to the fullest, complete and without regret.
References
- National Comprehensive Cancer Network Clinical Oncology Guidelines (NCCN GuidelinesR)
http://www.nccn.org/professionals/physician_gls/f_guidelines.asp accessed May 20,2015 - Health facts : Ministry of Health Malaysia Virtual Library
http://vlib.moh.gov.my/cms/content.jsp?id=com.tms.cms.section.Section_35… accessed May 20, 2015
Cancer Screening : What You Need to Know Before you Start – The Star, 28 June 2015.
Share:
Was this article helpful?
06 July 2015
•6 minute read
Cancer Screening - What You Need to Know Before You Start
Articles and Video
Learn more about General Surgery in Columbia Asia
Learn MoreShare:
Was this article helpful?
Health Packages
Elevate your health with tailored health packages at Columbia Asia Hospital. Take charge of your health journey today.
Pink October 2024
From
RM80
Pink October 2025
From
RM80
12.12 CheckJer Health Package
RM140
Find Out MoreColumbia Asia 30th Anniversary Promotion “Maternity & Baby”
HLA Policyholders Promo: Influenza Vaccination
RM65
Find Out More